Three graduates from QF’s medical school recount their experiences of treating COVID-19 patients in hospitals in the United States, which has witnessed the largest number of cases in the world.

In early March, Diala Steitieh was working her regular night shift at the NewYork-Presbyterian Hospital in Manhattan when she received a patient in his thirties with severe breathing difficulty and dry coughing.
The man did not have any pre-existing medical conditions, but had recently returned from a trip to Europe. Steitieh and her colleagues soon realized that the hospital had received its first COVID-19 patient and sprang into action, despite the fact there was no existing protocol for treatment of the new disease.
Steitieh, Resident Physician at the hospital and a graduate of Weill Cornell Medicine-Qatar (WCM-Q), one of Qatar Foundation’s international partner universities, recalls:
Everyone was very cautious. We had at least three physicians, fully gowned and protected to transfer him, with double gloves, a N95 mask, and an additional mask over that for protection of the eyes.’
Shortly after the first patient, Steitieh found herself in the middle of a global pandemic that would soon transfer New York City into one of the epicenters of the coronavirus outbreak.
Over the course of two weeks, we went from having one patient in one night to having multiple patients overnight. So it was a very stark and sudden increase in the number of cases,’

A few miles north of NewYork-Presbyterian, another WCM-Q graduate witnessed a similar progression of the crisis. Ali Khairat, a third-year Emergency Medicine Resident at the NYC Health + Hospitals/Lincoln saw his hospital transformed as the coronavirus outbreak unfolded in the city.
The rooms for non-urgent patients were converted into coronavirus-only wards, isolation rooms were activated, and the center witnessed a huge influx of patients with respiratory problems.
We have patients coming in with respiratory complaints, asthma, shortness of breath, and fever. We move them to the isolation room, protect ourselves with protective gear, and start interviewing the patient.
Since the start of the crisis, the situation in hospitals across the US has become more dire. Due to a shortage of personal protective equipment, healthcare professionals no longer have the luxury of following the standard procedure of changing masks and gowns for every new patient.
Siyab Panhwar, a WCM-Q alumnus who works as a cardiology fellow at Tulane Medical Center in Louisiana, another US state seriously affected by the pandemic, said:
We show up every day for work and can only pray that, this time around, the protective equipment will work. We are humans too, and we can also die. The lack of personal protective equipment is not ideal, but we just hope for the best when dealing with patients.’
According to Khairat, doctors are changing their ways of working to reduce the number of interactions with the COVID-19 patients.
We try to limit the number of healthcare providers interacting with the patients, so I have to go in to see the patient with everything I need to swab the person, make sure I get the complete medical history, do all the physical exams, and everything else that needs to be done happens in that one single interaction.’
Unfortunately, despite various safety measures, Khairat was infected with the virus and tested positive for COVID-19 in mid-March.
I started developing mild symptoms and was asked to go home. It took five days for my test results to come back, but by that time thankfully I was already feeling better.’
Khairat is currently recovering under self-quarantine at home, but anxiously waiting to be able to get back to work.
If a physician is exposed and starts showing symptoms, and has to be pulled out of the hospital, that’s a huge strain on the system. We are understaffed and have a limited number of residents. and losing one senior resident in the team can be incapacitating to the department.’
Since the coronavirus outbreak struck, Khairat, Panhwar, and Steitieh have all worked extra hours and given up their days off to meet the demands placed on frontline healthcare workers.
Steitieh said:
At any given day, about 10 physicians might not be able to come because they have either tested positive, have shown mild symptoms, or were unexpectedly exposed to patients with COVID-19. But I guess what makes it easier is that you are needed.’
Another key challenge for healthcare workers dealing with COVID-19 is that it is a novel virus with no set instructions regarding treatment or exactly how it affects the patient’s body.
Panhwar said:
There is no protocol, and whatever we know changes every day. In fact, it changes every hour. There is so much new information that’s coming in. This is something no one could have prepared for.’
Khairat adds:
All the evidence is anecdotal at best. There are a lot of grey areas, which are never a good thing in medicine. We have a responsibility to these patients, and it’s sobering and scary to be not able to give answers.’
The pandemic has posed unprecedented challenges to healthcare workers around the world, who are risking their lives to fight it. Yet Khairat, Panhwar, and Steitieh said their commitment to continue fighting the virus outweighs any personal concerns, adding that their medical education and residency experience have equipped them to be on the frontline.
Khairat said:
Being given all these tools through college and medical residency, and to actually apply them during a time when the world really needs you, is humbling and rewarding. It makes you feel you are participating in a human cause. ‘
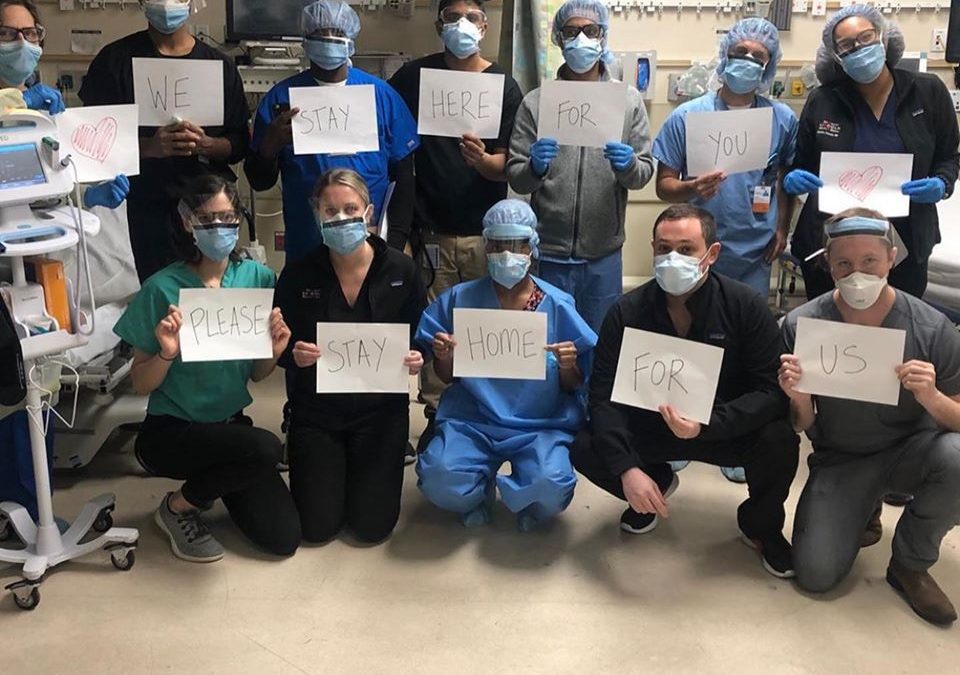
As the coronavirus continues to spread around the world, hospitals and medical staff remain overburdened. According to Panhwar, the public can help the situation by staying at home and reducing the number of cases — what is referred to as ‘flattening the curve.’

Panhwar says that the best cure is to not get it. He has now started documenting his experience on social media channels to highlight the importance of social isolation and other protective measures.
What I am trying to do on social media is to promote the fact that if you have to stay at home, stay at home. The public maybe don’t know the seriousness of the issue unless they actually see it from someone’s perspective who is treating these patients.’
Steitieh, who echoes the importance of following advice from healthcare and government leaders, said what helps her during these difficult times is the fact that people have been messaging her—both from within the US as well as from Qatar, where Steitieh and her family reside—to check in on her and appreciate her efforts.
I feel like, for the first time, medicine is the focus now. Before now, very infrequently did people talk about the number of hours that physicians put into work, even outside of a crisis like this. It’s been very heartwarming for all of us in medicine, and it makes it a lot easier to realise that you are appreciated for the time and effort you are putting in, and the risks you are taking.’